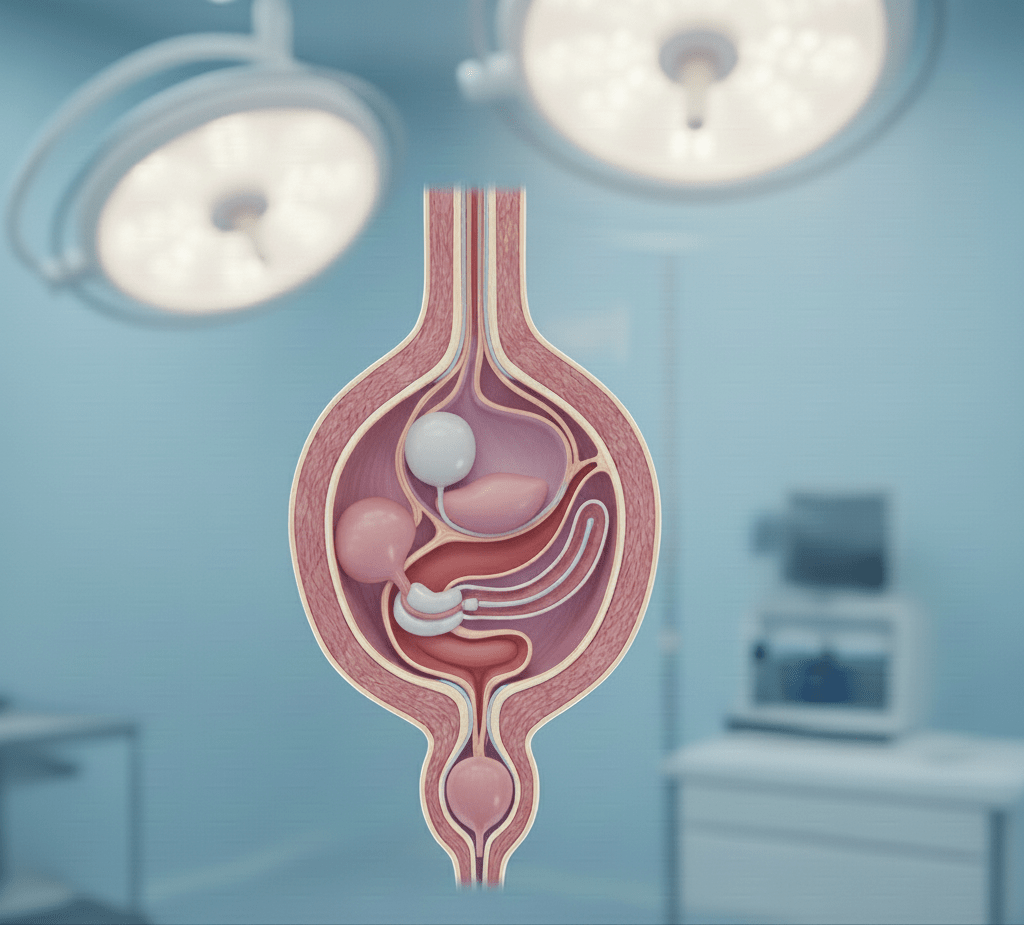
Placement of an artificial urinary sphincter
What is this gesture?
The artificial urinary sphincter (AUS) is an implantable device that replaces or supplements the function of the natural sphincter when it fails. It consists of three main parts: an inflatable cuff surrounding the urethra, a control pump (hand pump) and a reservoir balloon. When activated, the device compresses the urethra to prevent urine leakage. To urinate, the patient activates the pump, freeing the urethra for the time required, before the system automatically closes again.
This procedure is particularly indicated in cases ofpost-prostatectomy incontinence (urinary incontinence after prostate surgery), when stress urinary leaks are severe and persist despite well-managed rehabilitation. It is considered the reference treatment in this situation.

In which cases?
Indications
When an artificial urinary sphincter is proposed:
- Severe to major urinary incontinence after prostate surgery (radical prostatectomy), or after prostate interventions, if pelvic floor re-education is not sufficient.
- Significant stress urinary leakage, or copious leakage (often >300-500 mL/24h) depending on the case.
- Patient’s ability to manipulate the hand-controlled pump (skill, dexterity, understanding) to trigger micturition.
- Sterile urine, no urinary tract infection at the time of surgery.
- Favourable skin condition, good healing expected, no major antecedents that contraindicate the procedure (e.g. chronic infection, healing problems).
Surgical technique & procedure
Here is a typical procedure for artificial sphincter placement:
1️⃣ Pre-operation preparation
- Clinical assessment: urodynamics, flowmetry, assessment of post-micturition residual, urethral examination (endoscopy) to rule out any obstruction.
- Urinalysis to ensure absence of infection.
- Information and consent, explanation of the device, handling and post-operative procedures.
2️⃣ Surgery
- Anaesthesia: general or regional, depending on the patient.
- Incisions: often one at the perineum, one at the inguinal fold or in the abdominal region, depending on the type of sphincter used. Sometimes via the scrotal route in men.
- Place the cuff around the urethra, position the reservoir balloon and pump. The components are connected and the system is closed.
- The sphincter is left deactivated for the healing period (often several weeks) before being put into service.
3️⃣ Hospitalization and aftercare
Expected results & efficiency
- The rate of complete continence (no leakage) or social continence (very minimal acceptable leakage) is high: many series report perfect continence in ~75% of cases, and significant improvement in most others.
- Very good patient satisfaction, especially after failure of other solutions (rehabilitation, strips, etc.).
- Device service life: although mechanical, components may need to be overhauled or replaced over the years (pump, sleeve, leaks, wear).

Why choose this technique? The benefits
✔ Reference treatment for severe post-prostatectomy incontinence, often the most reliable when other solutions fail.
✔ Enables significant continence, improved quality of life.
✔ Fully implantable device: aesthetic, discreet, no visible or bulky external hardware.
Limits / risks , Contraindications & precautions
Limits / risks :
Contraindications & precautions
- Untreated active urinary tract infection.
- Poor skin or tissue condition around the implant (wounds, severe radiotherapy, poor vascularization).
- Patient unable to understand or manipulate the device (pump).
- Severe uncorrected disorders of the lower urinary tract (e.g. untreated urethral stenosis) or persistent obstruction.
Specialist in urological surgery
Prof. François Haab has experience in advanced urological surgery, including the placement of artificial sphincters.
✔ Ability to manage patients after prostatectomy, with all stages: assessment, implant choice, surgery, activation, follow-up.
✔ Personalized approach: taking into account the patient's history (radiotherapy, etc.), motor skills, dexterity, requests and expectations.
✔ Commitment to minimizing risk and ensuring optimal quality of life after surgery.
My journey in video
I made this video to introduce myself and describe my background and expertise.
Make an appointment
I welcome you to my Paris practice to discuss your expectations and propose the most appropriate solution: medical penoplasty or surgical penoplasty.
